5 Common Misconceptions About Fibroids and Their Treatment Options
A diagnosis of fibroids is worrisome for any woman.
It can also raise a lot of questions: Will fibroids cause infertility? Will fibroids affect pregnancy? Can fibroids turn into cancer? What are the treatment options for fibroids?
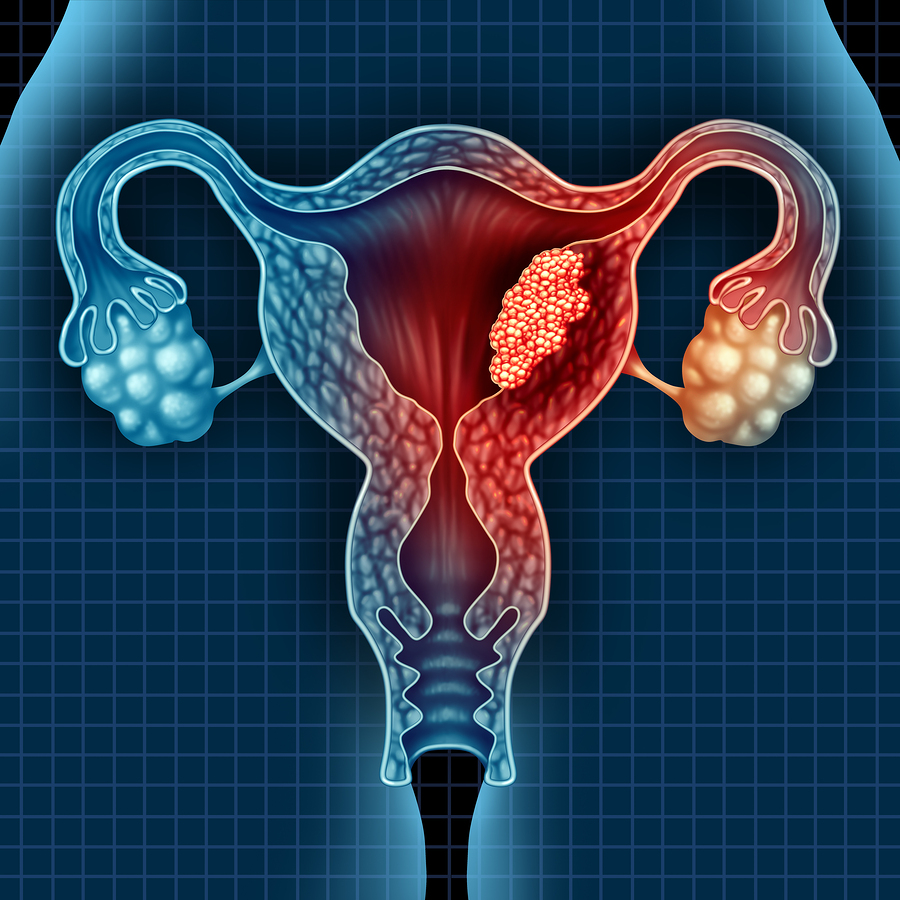
The first thing to impress upon a woman with fibroids is that this condition is common: anywhere from 75 to 80% of women will be diagnosed with uterine fibroids at some point in their lives. Fibroids often develop during the reproductive years, in women in their 20s and 30s. They can range in quantity, size and growth rate. They are most often noncancerous.1
Hearing all that is one thing, but when it’s your body, it’s not easy to dismiss fibroids as “nothing to be concerned about.” When it comes to a woman’s uterus during child-bearing years, an abnormal growth is worrisome, and misunderstandings often arise that can add to the worry.
In terms of patient care then, addressing those misconceptions is key to treatment and recovery. There are common misconceptions when it comes to treating fibroids, and we are going to address those five misconceptions and provide the facts, so patient care can proceed with less apprehension.
Here are 5 common misconceptions about fibroids and their treatment options.
Misconception #1: All Fibroids are Symptomatic
Many people believe that you need to have side effects to have a medical condition. If you have a cold, you have sneezing, coughing and a runny nose. So if you have fibroids, there must be symptoms, right?
Not so fast.
The reality is that many women have uterine fibroids without knowing it, because they don’t exhibit any symptoms. Fibroids are often discovered by accident when a doctor is doing a pelvic exam, an ultrasound, or some other examination.1
There’s also a big variation when it comes to fibroids:1
- Some are as small as seedlings, undetectable by the human eye1
- Some are bulky masses that can distort and enlarge the uterus1
- Some women have only one fibroid1
- Some women have multiple fibroids1
- Some women have so many fibroids that they expand the uterus, pushing out to the rib cage and adding weight to a woman’s body1
- Some fibroids form inside the uterus, while others may grow on its outer surface or within its wall, or be attached to the uterus by a stem-like structure2
- A fibroid may remain very small for a long time and suddenly grow rapidly, or grow slowly over a number of years2
If symptoms do present, here are the most common side effects:2
1. Changes in menstruation: longer, more frequent, or heavy menstrual periods; bleeding from the vagina at times other than during menstruation; anemia from blood loss.
2. Atypical pain: this can present as dull, heavy and aching, or sharp pain, in the abdomen or lower back; pain during sex.
3. Increased pressure in the lower body: this can result in frequent urination or difficulty urinating; abdominal cramps; or constipation, rectal pain, or difficult bowel movements.
4. Enlarged uterus and abdomen
5. Miscarriages
6. Infertility
There are instances when fibroids cause atypical symptoms too. One study cited a woman who visited emergency with her main complaint being pain in her lower abdomen region that had lasted seven days. The pain was nonradiating and had increased progressively, and she also had a low-grade fever. However, she had no menstrual complaints, and had regular menstrual cycles with average blood flow. Examination revealed a large fibroid.3
Since symptoms may not be present, or some of the side effects may be similar to other pelvic conditions—endometriosis is one example of a condition that can also cause painful intercourse, cramping, miscarriage or infertility—patient evaluation and diagnosis is key.
There are different pelvic examinations that can be used to diagnose fibroids. As mentioned, fibroids are sometimes found during routine visits to the doctor, or while being examined for something else, such as during a prenatal ultrasound.1
Otherwise, tests include an ultrasound, a special ultrasound called a saline hysterosonography, or an MRI. Other more specialized tests are conducted to confirm the diagnosis and to guide treatment options.4
One such procedure is a hysteroscopy, which lets a doctor or surgeon look inside the uterus to diagnose and treat fibroids and other conditions. A hysteroscopy is done using a hysteroscope, a thin, lighted tube that’s inserted into the vagina to examine the cervix and the inside of the uterus. An operative hysteroscopy is when fibroids or other adhesions like polyps are removed.5
The Benesta Hysteroscope made by Caldera Medical, for instance, can be used to view the uterine cavity for the purpose of diagnosis, as well as for surgical procedures. The accompanying Benesta Tissue Removal Device is a sterile, single-use hand-held device that is used to hysteroscopically remove intrauterine tissue. Used together, the Hysteroscope allows for visualizing the uterine cavity while performing hysteroscopy procedures with the Benesta Tissue Removal Device.
Caldera Medical focuses solely on women’s pelvic health, developing and building best-in-class surgical products for a variety of pelvic health issues, including fibroids. These products are used by surgeons worldwide.
Misconception #2: Surgery is the Only Effective Treatment
Once fibroids have been diagnosed, women often believe they must have surgery to remove them. That’s not the only solution for fibroid management.
Since up to 80 percent of women have fibroids before age 50, most women never need treatment of any kind. They may not be a problem at all unless they cause symptoms.6
Factors that influence treatment options include the age at which fibroids develop—when women develop fibroids at a young age, they have more time to grow and may be more likely to cause symptoms—as well as the size, number and location of fibroids.6
The most common symptoms are pressure on other organs and bleeding problems caused by fibroids. It’s very rare that cancer is a concern—one estimate states that in women with uterine masses that are causing symptoms, just one in every 200 to 500 is a cancerous tumor. The rest are fibroids.6
For the many fibroids that don’t require surgery, there are alternative treatment options that can be very successful:
1. Watch and wait: If symptoms are not present, or are not an issue, some women decide they can live with the fibroids, and monitor them over time. Age may be a factor, since fibroids tend to shrink after menopause, when levels of reproductive hormones drop.7
2. Medication: There are a variety of medications that can be used for treating the symptoms of uterine fibroids. For instance, medicine that targets the hormones that regulate menstrual cycles may relieve symptoms such as heavy menstrual bleeding and pelvic pressure.7
3. Embolization: In this medical procedure, small particles called embolic agents are injected into the arteries supplying the uterus. This will cut off the blood flow to fibroids, causing them to shrink and die.7
4. Ablation: This procedure uses radiofrequency energy to destroy uterine fibroids and shrink the blood vessels that feed them. This can be done during a laparoscopic or transcervical procedure. A similar procedure called cryomyolysis freezes the fibroids.7
These are just a few examples of options for treatment that don’t involve surgery. A hysterectomy to remove the uterus is a permanent solution for uterine fibroids, but it brings the end of a woman’s ability to get pregnant, and can bring on menopause.7
Each patient should have an individualized treatment plan, based on their symptoms, age, and personal preferences. Fibroids rarely interfere with pregnancy, but a woman’s desire to get pregnant may be part of the treatment plan.7
Treatments other than surgery can be very successful. Uterine fibroid embolization, for instance, is minimally invasive, requires minimal or no hospital stay, and has a shorter recovery than surgery, with an approximate success rate of 85%.8
Misconception #3: Fibroids Always Recur After Treatment
For those patients who are considering non-surgical treatments, there is a common fear that fibroids will return. That’s possible even with a surgery option such as a myomectomy, which removes the fibroids while keeping the uterus intact.9
A myomectomy removes current fibroids, but new fibroids can grow after you have a myomectomy, so it’s not always a permanent solution for fibroids. When this happens, the doctor may recommend a hysterectomy to prevent future growths.9
It seems that younger patients and those with more fibroids at the time of myomectomy are more likely to develop fibroids again in the future. Women nearing menopause are the least likely to have recurring problems from fibroids after a myomectomy.10
One study found no correlation between the time to reoperation for fibroids and race, number of fibroids, or aggregate weight. Other studies cited recurrence rates with a single fibroid was 9.5% vs 24.9% with multiple myomectomy. The same study stated that about 15–33% of fibroids recur after myomectomy, and around 10%-21% of women undergo a hysterectomy within five to ten years.11
A hysterectomy removes the uterus and so has serious implications—the patient cannot get pregnant, and if the ovaries are also removed, she will go into menopause.12
Another study compared women who received one of three treatments for fibroids: ablation; embolization and myomectomy. All three of these treatments try to save as much of the uterus as possible, and the study looked at how well the treatments delayed new or recurring symptoms and helped patients avoid follow-up treatments.13
Here are the results:13
- All three treatments worked about the same to prevent or delay new or recurring symptoms.
- Both uterine artery embolization and myomectomy were somewhat better than endometrial ablation at helping patients avoid follow-up treatments.
Misconception #4: Hysterectomy is the Definitive Cure
As we have already discussed, a hysterectomy will remove uterine fibroids, but only because it involves removing the entire uterus. A supracervical hysterectomy removes the upper part of the uterus, while a complete hysterectomy also includes removing the ovaries and cervix.9
There are certain risks and consequences:9
- A longer recovery time of up to eight weeks.
- A complete hysterectomy can bring on menopause.
- The surgery requires a hospital stay and general anesthesia.
- The woman can no longer get pregnant or carry a baby because she has no womb.
- A hysterectomy can cause damage to nearby organs and blood vessels.
- wound infections can occur along with a fever.
- Incontinence can become a problem after a hysterectomy. If the cervix is removed, it no longer supports the bladder and bowel, which can cause them to sink. Some women may notice pressure in the abdomen that they didn’t have before. There is also a greater risk of prolapse, organs moving down to the pelvic floor.
These implications must be discussed with the patient, who may want to explore alternatives that will spare the uterus while still dealing with fibroids. Age, number and size of fibroids, wanting to get pregnant, avoiding major surgery and desire for natural menopause are all considerations for the patient.
Misconception #5: Small Fibroids are Insignificant
While women are encouraged not to worry about fibroids—since they aren’t associated with an increased risk of uterine cancer and almost never develop into cancer—that doesn’t mean they should be ignored.1
In particular, women should seek medical attention if they have severe vaginal bleeding or sharp pelvic pain that comes on suddenly. Other symptoms of concern include pelvic pain that doesn’t go away; overly heavy, prolonged or painful periods; spotting or bleeding between periods; difficulty emptying the bladder; and anemia, or an unexplained low red blood cell count.1
Dealing with smaller fibroids may provide the following benefits:
- avoiding any future impact of fibroids on fertility and overall quality of life
- the ability to treat them with minimally invasive options
- better patient outcomes with early intervention
For instance, one study stated that there was a lower rate of second surgery when a “meticulous open technique” was used where even small palpable fibroids are removed before they have time to grow larger. It concluded that it was important to identify and remove small fibroids to prevent them from growing to a size that may later cause symptoms.11
While most uterine fibroids don’t cause serious complications, there is a chance of more concerning complications. Unmanageable pain, swelling of the abdomen or pelvic area, excessive bleeding that leads to anemia and risks to fertility are all reasons to deal with fibroids when they are diagnosed.12
Conclusion
Like many health conditions, open communication and patient education are vital to developing a treatment plan. The more doctors understand about fibroids, and pass that information on their patients, the better the outcome of any treatment plan.
The five misconceptions can be dispelled by obstetricians and gynecologists, improving patient care and empowering women with fibroids to choose the best option for their situation.
Women’s Pelvic Health issues are often not talked about due to embarrassment or lack of knowledge, leading women to believe they are alone on this journey. Whether you’re a woman suffering with fibroids or you’re treating someone with this condition, it’s important to remember that you’re not the only one. Don’t go through this journey alone.
There’s plenty of support, guidance and treatment options, including minimally invasive treatments offered by Caldera Medical, to help women regain confidence and live life to the fullest.